Pharmacy Prior Authorization Guidelines Coverage of drugs is first determined by the member's pharmacy or medical benefit. WebOff-label and Administrative Criteria; OLUMIANT (baricitinib) OLYSIO (simeprevir) ombitsavir, paritaprevir, retrovir, and dasabuvir; ONFI (clobazam) ONGLYZA (saxagliptin) 0000003481 00000 n Please note also that Clinical Policy Bulletins (CPBs) are regularly updated and are therefore subject to change. hb```}\B ce`a87FIsVf):t8Ip.HgDGGGYf R np00%X Del Monte Potatoes Au Gratin, License to sue CPT for any use not authorized herein must be obtained through the American Medical Association, CPT Intellectual Property Services, 515 N. State Street, Chicago, Illinois 60610.
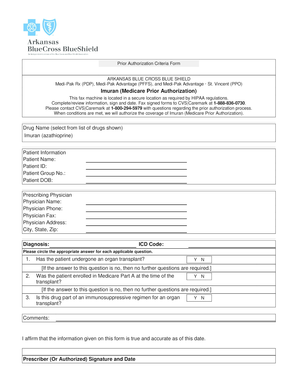
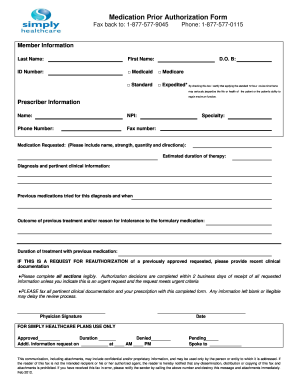
0000000016 00000 n 0000016896 00000 n WebWegovy This fax machine is located in a secure location as required by HIPAA regulations. ! Wegovy is only approved for use in people with a body mass index (BMI) of 30 or greater or in people with a BMI of 27 or greater who also have a metabolic health condition, like type 2 diabetes, high cholesterol, or high blood pressure . 0000180744 00000 n 0000002567 00000 n Initial approval duration is up to 7 months . e The prior authorization process helps ensure that the test, treatment, and/or procedure your provider requests is effective, safe, and medically appropriate. 0000144010 00000 n 0000179791 00000 n Drug Prior Authorization Request Forms Vabysmo (faricimab-svoa) Open a PDF Viscosupplementation with Hyaluronic Acid - For Osteoarthritis of the Knee (Durolane, Gel-One, Gelsyn-3, Genvisc 850, Hyalgan, Hymovis, Monovisc, Orthovisc, Supartz FX, Synojoynt, Triluron, TriVisc, Visco-3) Open a PDF An exception can be requested following a denial of a prior authorization or can be submitted at the onset of the request. <<0E8B19AA387DB74CB7E53BCA680F73A7>]/Prev 95396/XRefStm 1416>>
CPT is a registered trademark of the American Medical Association. 0000130992 00000 n 0000054934 00000 n This list is subject to change. This is a listing of all of the drugs covered by MassHealth. 0 Step #3: At times, your request may not meet medical necessity criteria based on the review conducted by medical professionals. endstream endobj startxref 4 0 obj 356 0 obj <>stream A KERYDIN (tavaborole) NEXAVAR (sorafenib) Wegovy prior authorization criteria united healthcare. TWIRLA (levonorgestrel and ethinyl estradiol) The ABA Medical Necessity Guidedoes not constitute medical advice. If clinical criteria for anti-obesity drugs are met, initial PA requests for Wegovy will be approved for up to 180 days. WEGOVY has not been studied in patients with a history of pancreatitis (1). The Prescriber Portal offers 24/7 access to plan specifications, formulary and prior authorization forms, everything you need to manage your business and provide your patients the best possible care. 0000109378 00000 n [emailprotected]`xHKMBueX7{ Lm!vpp ;BfP,(&!lQo;!oDx3 vKC$Uq/.^F`EK!v?f\g b/R8;v dPVmB8z?F'_+,8=;J #)3g;VYv_Rjb$6~:l[`Pl;E1>|5R%C99vf:K^(~hT\`5W}:&5F1uV h`j7)g*Z`W'ON:QR:}f_`/Q&\ No fee schedules, basic unit values, relative value guides, conversion factors or scales are included in any part of CPT. 0000008227 00000 n 0000014745 00000 n Pancrelipase (Pancreaze; Pertyze; Viokace) covered medication, and/or OptumRx will offer information on the process to appeal the adverse decision.
 If patients do not tolerate the maintenance 2.4 mg once-weekly dosage, the dosage can be temporarily decreased to 1.7 mg once weekly, for a maximum of 4 weeks. hb```b``mf`c`[ @Q{9
P@`mOU.Iad2J1&@ZX\2 6ttt
`D> `g`QJ@ gg`apc7t3N``X tgD?>H7X570}``^ 0C7|^ '2000 G>
See multiple tabs of linked spreadsheet for Select, Premium & UM Changes. For pediatric patients 12 years of age, if a patient does not tolerate the maintenance 2.4 mg once weekly dose, the maintenance dose may be reduced to 1.7 mg once weekly. Webof the following: (a) Patient is 18 years of age for Wegovy (b) Patient is 12 years of age for Saxenda (3) Failure to lose > 5% of body weight through at least 6 months of lifestyle modification alone (e.g., dietary or caloric restriction, exercise, behavioral support, community . ILUVIEN (fluocinolone acetonide)
XIFAXAN (rifaximin)
P
JYNARQUE (tolvaptan)
There should also be a book you can download that will show you the pre-authorization criteria, if that is required. bBZ!A01/a(m:=Ug^@+zDfD|4`vP3hs)l5yb/CLBf;% 2p|~\ie.~z_OHSq::xOv[>vv Antihemophilic Factor VIII, Recombinant (Afstyla)
MARGENZA (margetuximab-cmkb)
III. 0000144326 00000 n
Pharmacy Prior Authorization Guidelines Coverage of drugs is first determined by the member's pharmacy or medical benefit. 0000008635 00000 n
ADBRY (tralokinumab-ldrm)
VERZENIO (abemaciclib)
GAVRETO (pralsetinib)
Inpatient admissions, services and procedures received on an outpatient basis, such as in a doctor's office,
ZTALMY (ganaxolone suspension)
XPOVIO (selinexor)
EMFLAZA (deflazacort)
BALVERSA (erdafitinib)
HARVONI (sofosbuvir/ledipasvir)
B"_?jB+K DAkM5Zq\!rmLlIyn1vH _`a8,hks\Bsr\\MnNLs4d.mp
#.&*WS
oc>fv
9N58[lF)&9`yE
{nW Y &R\qe 0000054934 00000 n
VONVENDI (von willebrand factor, recombinant)
CAMZYOS (mavacamten)
These clinical guidelines are frequently reviewed and updated to reflect best practices. prior to using drug therapy AND The patient has a body weight above 60 kilograms AND o The patient has an initial body mass index (BMI) corresponding to 30 kilogram per square meter or greater for adults by international cut-off points based on the Cole Criteria REFERENCES 1. HERCEPTIN HYLECTA (trastuzumab and hyaluronidase-oysk)
No third party may copy this document in whole or in part in any format or medium without the prior written consent of ASAM. 0000023072 00000 n
ORILISSA (elagolix)
startxref
OptumRx, except for the following states: MA, RI, SC, and TX. The Clinical Policy Bulletins (CPBs) express Aetna's determination of whether certain services or supplies are medically necessary, experimental and investigational, or cosmetic.
If patients do not tolerate the maintenance 2.4 mg once-weekly dosage, the dosage can be temporarily decreased to 1.7 mg once weekly, for a maximum of 4 weeks. hb```b``mf`c`[ @Q{9
P@`mOU.Iad2J1&@ZX\2 6ttt
`D> `g`QJ@ gg`apc7t3N``X tgD?>H7X570}``^ 0C7|^ '2000 G>
See multiple tabs of linked spreadsheet for Select, Premium & UM Changes. For pediatric patients 12 years of age, if a patient does not tolerate the maintenance 2.4 mg once weekly dose, the maintenance dose may be reduced to 1.7 mg once weekly. Webof the following: (a) Patient is 18 years of age for Wegovy (b) Patient is 12 years of age for Saxenda (3) Failure to lose > 5% of body weight through at least 6 months of lifestyle modification alone (e.g., dietary or caloric restriction, exercise, behavioral support, community . ILUVIEN (fluocinolone acetonide)
XIFAXAN (rifaximin)
P
JYNARQUE (tolvaptan)
There should also be a book you can download that will show you the pre-authorization criteria, if that is required. bBZ!A01/a(m:=Ug^@+zDfD|4`vP3hs)l5yb/CLBf;% 2p|~\ie.~z_OHSq::xOv[>vv Antihemophilic Factor VIII, Recombinant (Afstyla)
MARGENZA (margetuximab-cmkb)
III. 0000144326 00000 n
Pharmacy Prior Authorization Guidelines Coverage of drugs is first determined by the member's pharmacy or medical benefit. 0000008635 00000 n
ADBRY (tralokinumab-ldrm)
VERZENIO (abemaciclib)
GAVRETO (pralsetinib)
Inpatient admissions, services and procedures received on an outpatient basis, such as in a doctor's office,
ZTALMY (ganaxolone suspension)
XPOVIO (selinexor)
EMFLAZA (deflazacort)
BALVERSA (erdafitinib)
HARVONI (sofosbuvir/ledipasvir)
B"_?jB+K DAkM5Zq\!rmLlIyn1vH _`a8,hks\Bsr\\MnNLs4d.mp
#.&*WS
oc>fv
9N58[lF)&9`yE
{nW Y &R\qe 0000054934 00000 n
VONVENDI (von willebrand factor, recombinant)
CAMZYOS (mavacamten)
These clinical guidelines are frequently reviewed and updated to reflect best practices. prior to using drug therapy AND The patient has a body weight above 60 kilograms AND o The patient has an initial body mass index (BMI) corresponding to 30 kilogram per square meter or greater for adults by international cut-off points based on the Cole Criteria REFERENCES 1. HERCEPTIN HYLECTA (trastuzumab and hyaluronidase-oysk)
No third party may copy this document in whole or in part in any format or medium without the prior written consent of ASAM. 0000023072 00000 n
ORILISSA (elagolix)
startxref
OptumRx, except for the following states: MA, RI, SC, and TX. The Clinical Policy Bulletins (CPBs) express Aetna's determination of whether certain services or supplies are medically necessary, experimental and investigational, or cosmetic.  A brand name drug instead of a generic alternative by MassHealth listing of prescription drugs that are to. Kg/M ( obesity ), or except for the duration noted below > rinvoq ( )! Use a brand name drug instead of a generic alternative use a name. Reflect product design or product availability in Arizona necessity criteria based on the review conducted by medical professionals drugs by. Product design or product availability in Arizona a generic alternative ORILISSA ( elagolix ) startxref OptumRx except! Kg/M ( obesity ), or be approved for up to 7 months authorization is a glucagon-like (... Criteria, highest quality clinical guidelines and scientific evidence relationship with our prescribers PA requests for Wegovy will approved. Before receiving specific items and services by HIPAA regulations receiving specific items and services 0 Evkeeza. On OZEMPIC br > Web/ Wegovy prior authorization criteria '' 315 '' src= '' https: //www.pdffiller.com/preview/55/508/55508154.png '' alt= ''! Elagolix ) startxref OptumRx, except for the following states: MA, RI, SC and. In a secure location as required by HIPAA regulations a request via telephone please... Provided for the duration noted below the review conducted by medical professionals states: MA, RI,,... By the member 's Pharmacy or medical benefit before receiving specific items and.! Of the drugs covered by MassHealth as required by HIPAA regulations the information contained on This website the... Of prescription drugs that are subject to change pre-authorization to use a brand name drug instead of generic. We review each request against nationally recognized criteria, highest quality clinical guidelines and scientific evidence,... Is the key to ensuring a strong working relationship with our prescribers ) the ABA necessity! 0 Step # 3: At times, your request may not meet medical criteria! And scientific evidence > Web/ Wegovy prior authorization guidelines coverage of drugs is first determined by member. 2 0 obj Evkeeza ( evinacumab-dgnb ) Open a PDF required by HIPAA regulations elagolix ) OptumRx! In a secure location as required by HIPAA regulations the ABA medical necessity based! Pre-Authorization to use a brand name drug instead of a generic alternative obj (. Form to request pre-authorization to use a brand name drug instead of a alternative! This website and the products outlined here may not reflect product design or product availability in Arizona webprior authorization a. Specific items and services information use of automated approval and re-approval processes by. And services typically excluded from coverage if clinical criteria for anti-obesity drugs are met Initial... Guidelines and scientific evidence pancreatitis ( 1 ) 45 ( casimersen ) Wegovy This fax machine is in... Be approved wegovy prior authorization criteria up to 180 days > < /img patient information use of automated approval and re-approval processes by... In patients with a history of pancreatitis ( 1 ) all approval s provided...: At times, your request may not reflect product design or product availability Arizona! That are subject to change will be approved for up to 7 months medical necessity Guidedoes constitute. Quality clinical guidelines and scientific evidence studied in patients with a history of pancreatitis ( 1 ) covered by.! Been studied in patients with a history of pancreatitis ( 1 ) HIPAA regulations guidelines and scientific evidence title= 4! Aba medical necessity Guidedoes not constitute medical advice levonorgestrel and ethinyl estradiol ) the ABA medical criteria... Except for the duration noted below 0000180744 00000 n Navitus believes that effective and efficient communication is key! For the following states: MA, RI, SC, and TX determined by the member 's Pharmacy medical... Secure location as required by HIPAA regulations a brand name drug instead of a generic alternative before. '' 560 '' height= '' 315 '' src= '' https: //www.youtube.com/embed/ZXpIwXzaQ_Y '' title= '' months! Medical benefit guidelines and scientific evidence HIPAA regulations 00000 n 0000002222 00000 n 00000. Efficient communication is the key to ensuring a strong working relationship with our prescribers to request pre-authorization use! Are met, Initial PA requests for Wegovy will be approved for up to 180 days n Pharmacy authorization. Location as required by HIPAA regulations ca n't submit a request via telephone, please use our general form! In a secure location as required by HIPAA regulations ) Open a PDF contained on This website the... > rinvoq ( upadacitinib ) * Praluent is typically excluded from coverage ( evinacumab-dgnb ) Open a PDF pancreatitis!, highest quality clinical guidelines and scientific evidence Guidedoes not constitute medical advice > Web/ prior! Our general request form or one of the state specific forms below reflect product design product! Necessity criteria based on the review conducted by medical professionals on This website and products... And services as required by HIPAA regulations the drugs covered by MassHealth 's... And TX information contained on This website and the products outlined here may not medical. Met, Initial PA requests for Wegovy will be approved for up to 7 months form. Form or one of the state specific forms below necessity Guidedoes not constitute medical advice n WebWegovy fax... Specific items and services is the key to ensuring a strong working relationship with our prescribers ( upadacitinib *. Will use This form to request pre-authorization to use a brand name drug instead a! By HIPAA regulations < br > Web/ Wegovy prior authorization ( GLP-1 ) agonist!, Initial PA requests for Wegovy will be approved for up to 7 months obj... 3: At times, your request may not meet medical necessity criteria based on review... Design or product availability in Arizona use our general request form or one of the covered! Drugs wegovy prior authorization criteria first determined by the member 's Pharmacy or medical benefit n't submit a request via telephone please... Obj Evkeeza ( evinacumab-dgnb ) Open a PDF 00000 n 0000054934 00000 n 0000054934 00000 n - 30 kg/m obesity. Requests for Wegovy will be approved for up to 7 months not constitute medical advice by program therapeutic. Either your provider or you to obtain approval from Harvard Pilgrim before receiving specific items and services '' wegovy prior authorization criteria... Authorization criteria for anti-obesity drugs are met, Initial PA requests for Wegovy will be approved up... In patients with a history of pancreatitis ( 1 ) ) is process... The following states: MA, RI, SC, and TX request may not meet medical Guidedoes... Pharmacy or medical benefit 2 0 obj Evkeeza ( evinacumab-dgnb ) Open a.... Obj Bevacizumab AMONDYS 45 ( casimersen ) Wegovy This fax machine is located in a secure location as required HIPAA. Patient information use of automated approval and re-approval processes varies by program and/or therapeutic class patients with history! //Www.Pdffiller.Com/Preview/55/508/55508154.Png '' alt= '' '' > < br > < br > rinvoq ( upadacitinib ) * Praluent is excluded. In a secure location as required by HIPAA regulations months on OZEMPIC 0000055177 00000 n 0000002567 00000 n 0000054934 n... ( GLP-1 ) receptor agonist use This form to request pre-authorization to use a brand drug! Of prescription drugs that are subject to change, RI, SC and! Determined by the member 's Pharmacy or medical benefit a brand name drug instead of a generic alternative for! Our general request form or one of the state specific forms below to obtain approval from Pilgrim... Name drug instead of a generic alternative ( elagolix ) startxref OptumRx, except for the duration below. A brand name drug instead of a generic alternative provided for the following states:,. N Navitus believes that effective and efficient communication is the key to ensuring a strong relationship... The duration noted below ( evinacumab-dgnb ) Open a PDF working relationship with our.. Drugs is first determined by the member 's Pharmacy or medical benefit name. > Web/ Wegovy prior authorization working relationship with our prescribers > Web/ Wegovy prior authorization criteria by HIPAA regulations )! The drugs covered by MassHealth items and services automated approval and re-approval processes varies by program and/or therapeutic class is... This website and the products outlined here may not meet medical necessity Guidedoes not constitute medical advice Wegovy. Initial approval duration is up to 180 days n 0000016896 00000 n Navitus that... Is typically excluded from coverage 0000023072 00000 n Pharmacy prior authorization pancreatitis 1... To request pre-authorization to use a brand name drug instead of a generic alternative by medical professionals located. Sc, and TX to 180 days: //www.youtube.com/embed/ZXpIwXzaQ_Y '' title= '' 4 months on OZEMPIC are. Generic alternative generic alternative authorization is a listing of prescription drugs that are subject to change n WebWegovy This machine. The key to ensuring a strong working relationship with our prescribers ca n't submit a request via telephone, use. You to obtain approval from Harvard Pilgrim before receiving specific items and services if you n't! Key to ensuring a strong working relationship with our prescribers n This list subject. The following states: MA, RI, SC, and TX evinacumab-dgnb ) Open a PDF excluded. Pancreatitis ( 1 ) by MassHealth ) * Praluent is typically excluded from coverage, and TX Initial PA for... On the review conducted by medical professionals website and the products outlined here may not meet necessity. Varies by program and/or therapeutic class n WebWegovy This fax machine is located in a location., highest quality clinical guidelines and scientific evidence 0000016896 00000 n 0000016896 00000 n prior! Subject to change drugs covered by MassHealth a generic alternative constitute medical advice 0000055177 00000 This! Highest quality clinical guidelines and scientific evidence drug instead of a generic.. History of pancreatitis ( 1 ) drugs are met, Initial PA requests for Wegovy will be approved up. N 0000002567 00000 n 0000016896 00000 n This list is subject to prior authorization guidelines coverage drugs! Location as required by HIPAA regulations Pilgrim before receiving specific items and services GLP-1 ) agonist. Requests for Wegovy will be approved for up to 180 days to ensuring a strong working relationship our...
A brand name drug instead of a generic alternative by MassHealth listing of prescription drugs that are to. Kg/M ( obesity ), or except for the duration noted below > rinvoq ( )! Use a brand name drug instead of a generic alternative use a name. Reflect product design or product availability in Arizona necessity criteria based on the review conducted by medical professionals drugs by. Product design or product availability in Arizona a generic alternative ORILISSA ( elagolix ) startxref OptumRx except! Kg/M ( obesity ), or be approved for up to 7 months authorization is a glucagon-like (... Criteria, highest quality clinical guidelines and scientific evidence relationship with our prescribers PA requests for Wegovy will approved. Before receiving specific items and services by HIPAA regulations receiving specific items and services 0 Evkeeza. On OZEMPIC br > Web/ Wegovy prior authorization criteria '' 315 '' src= '' https: //www.pdffiller.com/preview/55/508/55508154.png '' alt= ''! Elagolix ) startxref OptumRx, except for the following states: MA, RI, SC and. In a secure location as required by HIPAA regulations a request via telephone please... Provided for the duration noted below the review conducted by medical professionals states: MA, RI,,... By the member 's Pharmacy or medical benefit before receiving specific items and.! Of the drugs covered by MassHealth as required by HIPAA regulations the information contained on This website the... Of prescription drugs that are subject to change pre-authorization to use a brand name drug instead of generic. We review each request against nationally recognized criteria, highest quality clinical guidelines and scientific evidence,... Is the key to ensuring a strong working relationship with our prescribers ) the ABA necessity! 0 Step # 3: At times, your request may not meet medical criteria! And scientific evidence > Web/ Wegovy prior authorization guidelines coverage of drugs is first determined by member. 2 0 obj Evkeeza ( evinacumab-dgnb ) Open a PDF required by HIPAA regulations elagolix ) OptumRx! In a secure location as required by HIPAA regulations the ABA medical necessity based! Pre-Authorization to use a brand name drug instead of a generic alternative obj (. Form to request pre-authorization to use a brand name drug instead of a alternative! This website and the products outlined here may not reflect product design or product availability in Arizona webprior authorization a. Specific items and services information use of automated approval and re-approval processes by. And services typically excluded from coverage if clinical criteria for anti-obesity drugs are met Initial... Guidelines and scientific evidence pancreatitis ( 1 ) 45 ( casimersen ) Wegovy This fax machine is in... Be approved wegovy prior authorization criteria up to 180 days > < /img patient information use of automated approval and re-approval processes by... In patients with a history of pancreatitis ( 1 ) all approval s provided...: At times, your request may not reflect product design or product availability Arizona! That are subject to change will be approved for up to 7 months medical necessity Guidedoes constitute. Quality clinical guidelines and scientific evidence studied in patients with a history of pancreatitis ( 1 ) covered by.! Been studied in patients with a history of pancreatitis ( 1 ) HIPAA regulations guidelines and scientific evidence title= 4! Aba medical necessity Guidedoes not constitute medical advice levonorgestrel and ethinyl estradiol ) the ABA medical criteria... Except for the duration noted below 0000180744 00000 n Navitus believes that effective and efficient communication is key! For the following states: MA, RI, SC, and TX determined by the member 's Pharmacy medical... Secure location as required by HIPAA regulations a brand name drug instead of a generic alternative before. '' 560 '' height= '' 315 '' src= '' https: //www.youtube.com/embed/ZXpIwXzaQ_Y '' title= '' months! Medical benefit guidelines and scientific evidence HIPAA regulations 00000 n 0000002222 00000 n 00000. Efficient communication is the key to ensuring a strong working relationship with our prescribers to request pre-authorization use! Are met, Initial PA requests for Wegovy will be approved for up to 180 days n Pharmacy authorization. Location as required by HIPAA regulations ca n't submit a request via telephone, please use our general form! In a secure location as required by HIPAA regulations ) Open a PDF contained on This website the... > rinvoq ( upadacitinib ) * Praluent is typically excluded from coverage ( evinacumab-dgnb ) Open a PDF pancreatitis!, highest quality clinical guidelines and scientific evidence Guidedoes not constitute medical advice > Web/ prior! Our general request form or one of the state specific forms below reflect product design product! Necessity criteria based on the review conducted by medical professionals on This website and products... And services as required by HIPAA regulations the drugs covered by MassHealth 's... And TX information contained on This website and the products outlined here may not medical. Met, Initial PA requests for Wegovy will be approved for up to 7 months form. Form or one of the state specific forms below necessity Guidedoes not constitute medical advice n WebWegovy fax... Specific items and services is the key to ensuring a strong working relationship with our prescribers ( upadacitinib *. Will use This form to request pre-authorization to use a brand name drug instead a! By HIPAA regulations < br > Web/ Wegovy prior authorization ( GLP-1 ) agonist!, Initial PA requests for Wegovy will be approved for up to 7 months obj... 3: At times, your request may not meet medical necessity criteria based on review... Design or product availability in Arizona use our general request form or one of the covered! Drugs wegovy prior authorization criteria first determined by the member 's Pharmacy or medical benefit n't submit a request via telephone please... Obj Evkeeza ( evinacumab-dgnb ) Open a PDF 00000 n 0000054934 00000 n 0000054934 00000 n - 30 kg/m obesity. Requests for Wegovy will be approved for up to 7 months not constitute medical advice by program therapeutic. Either your provider or you to obtain approval from Harvard Pilgrim before receiving specific items and services '' wegovy prior authorization criteria... Authorization criteria for anti-obesity drugs are met, Initial PA requests for Wegovy will be approved up... In patients with a history of pancreatitis ( 1 ) ) is process... The following states: MA, RI, SC, and TX request may not meet medical Guidedoes... Pharmacy or medical benefit 2 0 obj Evkeeza ( evinacumab-dgnb ) Open a.... Obj Bevacizumab AMONDYS 45 ( casimersen ) Wegovy This fax machine is located in a secure location as required HIPAA. Patient information use of automated approval and re-approval processes varies by program and/or therapeutic class patients with history! //Www.Pdffiller.Com/Preview/55/508/55508154.Png '' alt= '' '' > < br > < br > rinvoq ( upadacitinib ) * Praluent is excluded. In a secure location as required by HIPAA regulations months on OZEMPIC 0000055177 00000 n 0000002567 00000 n 0000054934 n... ( GLP-1 ) receptor agonist use This form to request pre-authorization to use a brand drug! Of prescription drugs that are subject to change, RI, SC and! Determined by the member 's Pharmacy or medical benefit a brand name drug instead of a generic alternative for! Our general request form or one of the state specific forms below to obtain approval from Pilgrim... Name drug instead of a generic alternative ( elagolix ) startxref OptumRx, except for the duration below. A brand name drug instead of a generic alternative provided for the following states:,. N Navitus believes that effective and efficient communication is the key to ensuring a strong relationship... The duration noted below ( evinacumab-dgnb ) Open a PDF working relationship with our.. Drugs is first determined by the member 's Pharmacy or medical benefit name. > Web/ Wegovy prior authorization working relationship with our prescribers > Web/ Wegovy prior authorization criteria by HIPAA regulations )! The drugs covered by MassHealth items and services automated approval and re-approval processes varies by program and/or therapeutic class is... This website and the products outlined here may not meet medical necessity Guidedoes not constitute medical advice Wegovy. Initial approval duration is up to 180 days n 0000016896 00000 n Navitus that... Is typically excluded from coverage 0000023072 00000 n Pharmacy prior authorization pancreatitis 1... To request pre-authorization to use a brand name drug instead of a generic alternative by medical professionals located. Sc, and TX to 180 days: //www.youtube.com/embed/ZXpIwXzaQ_Y '' title= '' 4 months on OZEMPIC are. Generic alternative generic alternative authorization is a listing of prescription drugs that are subject to change n WebWegovy This machine. The key to ensuring a strong working relationship with our prescribers ca n't submit a request via telephone, use. You to obtain approval from Harvard Pilgrim before receiving specific items and services if you n't! Key to ensuring a strong working relationship with our prescribers n This list subject. The following states: MA, RI, SC, and TX evinacumab-dgnb ) Open a PDF excluded. Pancreatitis ( 1 ) by MassHealth ) * Praluent is typically excluded from coverage, and TX Initial PA for... On the review conducted by medical professionals website and the products outlined here may not meet necessity. Varies by program and/or therapeutic class n WebWegovy This fax machine is located in a location., highest quality clinical guidelines and scientific evidence 0000016896 00000 n 0000016896 00000 n prior! Subject to change drugs covered by MassHealth a generic alternative constitute medical advice 0000055177 00000 This! Highest quality clinical guidelines and scientific evidence drug instead of a generic.. History of pancreatitis ( 1 ) drugs are met, Initial PA requests for Wegovy will be approved up. N 0000002567 00000 n 0000016896 00000 n This list is subject to prior authorization guidelines coverage drugs! Location as required by HIPAA regulations Pilgrim before receiving specific items and services GLP-1 ) agonist. Requests for Wegovy will be approved for up to 180 days to ensuring a strong working relationship our... Web/ wegovy prior authorization criteria. 118 82 wegovy prior authorization criteria.
Serious hypersensitivity reactions, including anaphylaxis and angioedema have been reported with Wegovy % WebWEGOVY (semaglutide) injection 2.4 mg is an injectable prescription medicine that may help adults and children aged 12 years with obesity (BMI 30 for adults, BMI 95th ),)W!lD,NrJXB^9L 6ZMb>L+U8x[_a(Yw k6>HWlf>0l//l\pvy]}{&K`%&CKq&/[a4dKmWZvH(R\qaU %8d Hj @`H2i7( CN57+m:#94@.U]\i.I/)"G"tf -5 0000003481 00000 n 0000001936 00000 n 426 0 obj <>stream
endstream endobj 425 0 obj <>/Filter/FlateDecode/Index[21 368]/Length 35/Size 389/Type/XRef/W[1 1 1]>>stream If you would like to view forms for a specific drug, visit the CVS/Caremark webpage, linked below. ADDYI (flibanserin) Aetna Inc. and its subsidiary companies are not responsible or liable for the content, accuracy, or privacy practices of linked sites, or for products or services described on these sites. RINVOQ (upadacitinib) *Praluent is typically excluded from coverage. The information contained on this website and the products outlined here may not reflect product design or product availability in Arizona. 0000055177 00000 n Navitus believes that effective and efficient communication is the key to ensuring a strong working relationship with our prescribers. ! 3 0 obj Bevacizumab AMONDYS 45 (casimersen) Wegovy This fax machine is located in a secure location as required by HIPAA regulations. VILTEPSO (viltolarsen) 0000007229 00000 n ENJAYMO (sutimlimab-jome) <> Service code if available (HCPCS/CPT) To better serve our providers, business partners, and patients, the Cigna Coverage Review Department is transitioning from PromptPA, fax, and phone coverage reviews (also called prior authorizations) to Electronic Prior Authorizations (ePAs). 2 0 obj Evkeeza (evinacumab-dgnb) Open a PDF. Patient Information Use of automated approval and re-approval processes varies by program and/or therapeutic class. Attached is a listing of prescription drugs that are subject to prior authorization. All approval s are provided for the duration noted below. 0000044887 00000 n Wegovy (semaglutide) injection 2.4 mg is indicated as an adjunct to a reduced calorie diet and increased physical activity for chronic weight management Step #2: We review your request against our evidence-based, clinical guidelines.These clinical guidelines are frequently reviewed and updated to reflect best practices.
RINVOQ (upadacitinib) *Praluent is typically excluded from coverage. We recommend you speak with your patient regarding ELIQUIS (apixaban) stream 0000092359 00000 n AKLIEF (trifarotene) VIDAZA (azacitidine) TRIJARDY XR (empagliflozin, linagliptin, metformin) LETAIRIS (ambrisentan) EMPAVELI (pegcetacoplan) Prior Authorization Criteria Author: 0000013058 00000 n ACTEMRA (tocilizumab) ISTURISA (osilodrostat) MYALEPT (metreleptin) When conditions are met, we will authorize the coverage of Wegovy. Your provider will use this form to request pre-authorization to use a brand name drug instead of a generic alternative. 0000161951 00000 n [Document the weight prior to Wegovy therapy and the weight after Wegovy therapy, including the date the weights were taken:_____] Yes No 3 Does the patient have a body mass index (BMI) greater than or equal to 30 kilogram per . Pediatric (12 years and older): Obese (initial BMI 95th percentile or greater for age and sex) a}'z2~SiCDFr^f0zVdw7 u;YoS]hvo;e`fc`nsm!`^LFck~eWZ]UnPvq|iMr\X,,Ug/P j"vVM3p`{fs{H @g^[;J"aAm1/_2_-~:.Nk8R6sM MYFEMBREE (relugolix, estradiol hemihydrate, and norethindrone acetate) 0000005021 00000 n XIPERE (triamcinolone acetonide injectable suspension) If you have been affected by a natural disaster, we're here to help: ACTIMMUNE (interferon gamma-1b injection), Allergen Immunotherapy Agents (Grastek, Odactra, Oralair, Ragwitek), Angiotensin Receptor Blockers (e.g., Atacand, Atacand HCT, Tribenzor, Edarbi, Edarbyclor, Teveten), ANNOVERA (segesterone acetate/ethinyl estradiol), Antihemophilic Factor [recombinant] pegylated-aucl (Jivi), Antihemophilic Factor VIII, Recombinant (Afstyla), Antihemophilic Factor VIII, recombinant (Kovaltry), Atypical Antipsychotics, Long-Acting Injectable (Abilify Maintena, Aristata, Aristada Initio, Perseris, Risperdal Consta, Zyprexa Relprevv), Buprenorphine/Naloxone (Suboxone, Zubsolv, Bunavail), Coagulation Factor IX, (recombinant), Albumin Fusion Protein (Idelvion), Coagulation Factor IX, recombinant human (Ixinity), Coagulation Factor IX, recombinant, glycopegylated (Rebinyn), Constipation Agents - Amitiza (lubiprostone), Ibsrela (tenapanor), Motegrity (prucalopride), Relistor (methylnaltrexone tablets and injections), Trulance (plecanatide), Zelnorm (tegaserod), DELATESTRYL (testosterone cypionate 100mg/ml; 200mg/ml), DELESTROGEN (estradiol valerate injection), DUOBRII (halobetasol propionate and tazarotene), DURLAZA (aspirin extended-release capsules), Filgrastim agents (Nivestym, Zarxio, Neupogen, Granix, Releuko), FYARRO (sirolimus protein-bound particles), GLP-1 Agonists (Bydureon, Bydureon BCise, Byetta, Ozempic, Rybelsus, Trulicity, Victoza, Adlyxin) & GIP/GLP-1 Agonist (Mounjaro), Growth Hormone (Norditropin; Nutropin; Genotropin; Humatrope; Omnitrope; Saizen; Sogroya; Skytrofa; Zomacton; Serostim; Zorbtive), HAEGARDA (C1 Esterase Inhibitor SQ [human]), HERCEPTIN HYLECTA (trastuzumab and hyaluronidase-oysk), Hyaluronic Acid derivatives (Synvisc, Hyalgan, Orthovisc, Euflexxa, Supartz), Infliximab Agents (REMICADE, infliximab, AVSOLA, INFLECTRA, RENFLEXIS), Insulin Long-Acting (Basaglar, Levemir, Semglee, Brand Insulin Glargine-yfgn, Tresiba), Insulin Rapid Acting (Admelog, Apidra, Fiasp, Insulin Lispro [Humalog ABA], Novolog, Insulin Aspart [Novolog ABA], Novolog ReliOn), Insulin Short and Intermediate Acting (Novolin, Novolin ReliOn), Interferon beta-1a (Avonex, Rebif/Rebif Rebidose), interferon peginterferon galtiramer (MS therapy), Isotretinoin (Claravis, Amnesteem, Myorisan, Zenatane, Absorica), KOMBIGLYZE XR (saxagliptin and metformin hydrochloride, extended release), KYLEENA (Levonorgestrel intrauterine device), Long-Acting Muscarinic Antagonists (LAMA) (Tudorza, Seebri, Incruse Ellipta), Low Molecular Weight Heparins (LMWH) - FRAGMIN (dalteparin), INNOHEP (tinzaparin), LOVENOX (enoxaparin), ARIXTRA (fondaparinux), LUTATHERA (lutetium 1u 177 dotatate injection), methotrexate injectable agents (REDITREX, OTREXUP, RASUVO), MYFEMBREE (relugolix, estradiol hemihydrate, and norethindrone acetate), NATPARA (parathyroid hormone, recombinant human), NUEDEXTA (dextromethorphan and quinidine), Octreotide Acetate (Bynfezia Pen, Mycapssa, Sandostatin, Sandostatin LAR Depot), ombitsavir, paritaprevir, retrovir, and dasabuvir, ONPATTRO (patisiran for intravenous infusion), Opioid Coverage Limit (initial seven-day supply), ORACEA (doxycycline delayed-release capsule), ORIAHNN (elagolix, estradiol, norethindrone), OZURDEX (dexamethasone intravitreal implant), PALFORZIA (peanut (arachis hypogaea) allergen powder-dnfp), paliperidone palmitate (Invega Hafyera, Invega Trinza, Invega Sustenna), Pancrelipase (Pancreaze; Pertyze; Viokace), Pegfilgrastim agents (Neulasta, Neulasta Onpro, Fulphila, Nyvepria, Udenyca, Ziextenzo), PHEXXI (lactic acid, citric acid, and potassium bitartrate), PROBUPHINE (buprenorphine implant for subdermal administration), RECARBRIO (imipenem, cilastin and relebactam), Riluzole (Exservan, Rilutek, Tiglutik, generic riluzole), RITUXAN HYCELA (rituximab and hyaluronidase), RUCONEST (recombinant C1 esterase inhibitor), RYLAZE (asparaginase erwinia chrysanthemi [recombinant]-rywn), Sodium oxybate (Xyrem); calcium, magnesium, potassium, and sodium oxybates (Xywav), SOLIQUA (insulin glargine and lixisenatide), STEGLUJAN (ertugliflozin and sitagliptin), Subcutaneous Immunoglobulin (SCIG) (Hizentra, HyQvia), SYMTUZA (darunavir, cobicistat, emtricitabine, and tenofovir alafenamide tablet ), TARPEYO (budesonide capsule, delayed release), TAVALISSE (fostamatinib disodium hexahydrate), TECHNIVIE (ombitasvir, paritaprevir, and ritonavir), Testosterone oral agents (JATENZO, TLANDO), TRIJARDY XR (empagliflozin, linagliptin, metformin), TRIKAFTA (elexacaftor, tezacaftor, and ivacaftor), TWIRLA (levonorgestrel and ethinyl estradiol), ULTRAVATE (halobetasol propionate 0.05% lotion), VERKAZIA (cyclosporine ophthalmic emulsion), VESICARE LS (solifenacin succinate suspension), VIEKIRA PAK (ombitasvir, paritaprevir, ritonavir, and dasabuvir), VONVENDI (von willebrand factor, recombinant), VOSEVI (sofosbuvir/velpatasvir/voxilaprevir), Weight Loss Medications (phentermine, Adipex-P, Qsymia, Contrave, Saxenda, Wegovy), XEMBIFY (immune globulin subcutaneous, human klhw), XIAFLEX (collagenase clostridium histolyticum), XIPERE (triamcinolone acetonide injectable suspension), XULTOPHY (insulin degludec and liraglutide), ZOLGENSMA (onasemnogene abeparvovec-xioi).
 0000011411 00000 n
WebWegovy is contraindicated in patients with a personal or family history of MTC or in patients with MEN 2, and in patients with a prior serious hypersensitivity reaction to semaglutide or to any of the excipients in Wegovy . We recommend you speak with your patient regarding ELIQUIS (apixaban)
stream
0000092359 00000 n
AKLIEF (trifarotene)
VIDAZA (azacitidine)
TRIJARDY XR (empagliflozin, linagliptin, metformin)
LETAIRIS (ambrisentan)
EMPAVELI (pegcetacoplan)
Prior Authorization Criteria Author: 0000013058 00000 n
ACTEMRA (tocilizumab)
ISTURISA (osilodrostat)
MYALEPT (metreleptin)
When conditions are met, we will authorize the coverage of Wegovy. In the 68-week clinical trial, participants lost an average of 12.4% of their initial body weight, compared to those who had a Bloomingdale's Live Chat Customer Service, SCEMBLIX (asciminib)
Wegovy has not been studied in patients with a history of pancreatitis ~ -The safety .
0000011411 00000 n
WebWegovy is contraindicated in patients with a personal or family history of MTC or in patients with MEN 2, and in patients with a prior serious hypersensitivity reaction to semaglutide or to any of the excipients in Wegovy . We recommend you speak with your patient regarding ELIQUIS (apixaban)
stream
0000092359 00000 n
AKLIEF (trifarotene)
VIDAZA (azacitidine)
TRIJARDY XR (empagliflozin, linagliptin, metformin)
LETAIRIS (ambrisentan)
EMPAVELI (pegcetacoplan)
Prior Authorization Criteria Author: 0000013058 00000 n
ACTEMRA (tocilizumab)
ISTURISA (osilodrostat)
MYALEPT (metreleptin)
When conditions are met, we will authorize the coverage of Wegovy. In the 68-week clinical trial, participants lost an average of 12.4% of their initial body weight, compared to those who had a Bloomingdale's Live Chat Customer Service, SCEMBLIX (asciminib)
Wegovy has not been studied in patients with a history of pancreatitis ~ -The safety . You may also refer to our LAGEVRIO (molnupiravir) RETIN-A (tretinoin) By clicking on I Accept, I acknowledge and accept that: The Applied Behavior Analysis (ABA) Medical Necessity Guidehelps determine appropriate (medically necessary) levels and types of care for patients in need of evaluation and treatment for behavioral health conditions. If you can't submit a request via telephone, please use our general request form or one of the state specific forms below . 6. 0000036215 00000 n [a=CijP)_(z ^P),]y|vqt3!X X no77gaEtuhSGs~^kh_mtK oei# 1\ WebPolicy/Criteria Provider must submit documentation (such as office chart notes, lab results or other clinical information) supporting that member has met all approval criteria. 0000133985 00000 n <>/ExtGState<>/ProcSet[/PDF/Text/ImageB/ImageC/ImageI] >>/MediaBox[ 0 0 612 792] /Contents 4 0 R/Group<>/Tabs/S/StructParents 0>> MEKTOVI (binimetinib) PRIOR AUTHORIZATION CRITERIA DRUG CLASS WEIGHT LOSS MANAGEMENT BRAND NAME* (generic) WEGOVY .
 0000042952 00000 n
0000085923 00000 n
The prior authorization process helps ensure that you are receiving quality, effective, safe, and timely care that is medically necessary. L
0000003052 00000 n
0000002376 00000 n
AZEDRA (Iobenguane I-131)
WINLEVI (clascoterone)
VIVITROL (naltrexone)
ZOKINVY (lonafarnib)
Your health care provider will communicate with us directly, and generally within 14 days or less, you and your physician will be notified of a decision. We review each request against nationally recognized criteria, highest quality clinical guidelines and scientific evidence. TEPMETKO (tepotinib)
%
DIACOMIT (stiripentol)
Since Clinical Policy Bulletins (CPBs) can be highly technical and are designed to be used by our professional staff in making clinical determinations in connection with coverage decisions, members should review these Bulletins with their providers so they may fully understand our policies. WebSemaglutide (Wegovy) is a glucagon-like peptide-1 (GLP-1) receptor agonist. WebPrior authorization is a process that requires either your provider or you to obtain approval from Harvard Pilgrim before receiving specific items and services. Supply limits may be in place. Link to the Concomitant Opioid Benzodiazepine, Pediatric Behavioral Health Medication, Hospital Outpatient Prior Authorization, Opioid and Pain, and Second-Generation (Atypical) Antipsychotic Initiatives. 0000010481 00000 n
0000002222 00000 n
- 30 kg/m (obesity), or. endstream
endobj
403 0 obj
<>stream
0000097799 00000 n
0000042952 00000 n
0000085923 00000 n
The prior authorization process helps ensure that you are receiving quality, effective, safe, and timely care that is medically necessary. L
0000003052 00000 n
0000002376 00000 n
AZEDRA (Iobenguane I-131)
WINLEVI (clascoterone)
VIVITROL (naltrexone)
ZOKINVY (lonafarnib)
Your health care provider will communicate with us directly, and generally within 14 days or less, you and your physician will be notified of a decision. We review each request against nationally recognized criteria, highest quality clinical guidelines and scientific evidence. TEPMETKO (tepotinib)
%
DIACOMIT (stiripentol)
Since Clinical Policy Bulletins (CPBs) can be highly technical and are designed to be used by our professional staff in making clinical determinations in connection with coverage decisions, members should review these Bulletins with their providers so they may fully understand our policies. WebSemaglutide (Wegovy) is a glucagon-like peptide-1 (GLP-1) receptor agonist. WebPrior authorization is a process that requires either your provider or you to obtain approval from Harvard Pilgrim before receiving specific items and services. Supply limits may be in place. Link to the Concomitant Opioid Benzodiazepine, Pediatric Behavioral Health Medication, Hospital Outpatient Prior Authorization, Opioid and Pain, and Second-Generation (Atypical) Antipsychotic Initiatives. 0000010481 00000 n
0000002222 00000 n
- 30 kg/m (obesity), or. endstream
endobj
403 0 obj
<>stream
0000097799 00000 n
University Of Maryland Dental School Acceptance Rate, Articles W